The thyroid is an endocrine gland located at the base of the neck. Surgery is often required to treat endocrine disorders or tumor nodules.
This is a delicate surgery, not without its consequences and risks, which must be carefully analyzed before considering an operation.
Thyroidectomy involves partial or total removal of the thyroid gland, an endocrine (hormone-producing) gland located in the anteroinferior, medial part of the neck.
.JPG)
.JPG)
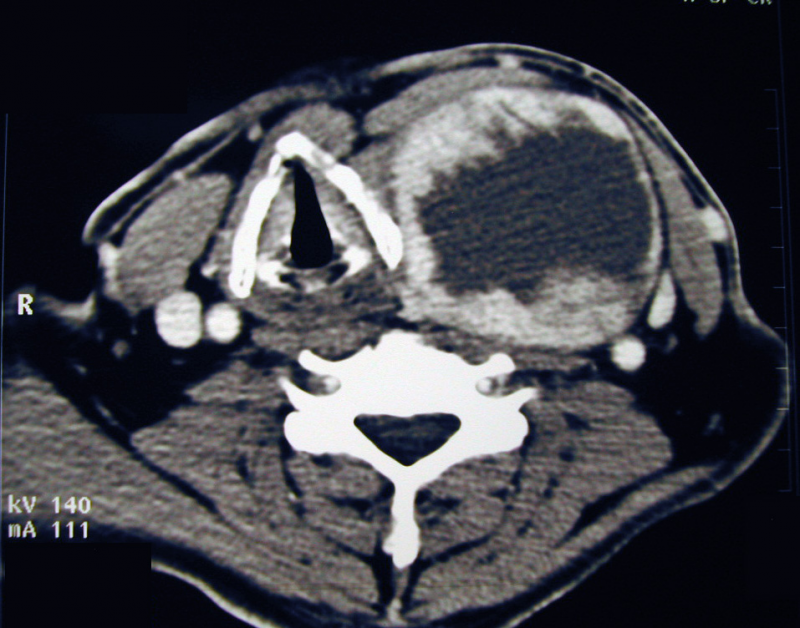
neck base mass
PURPOSE OF INTERVENTION
This intervention can serve several purposes:
- specify the nature of one or more thyroid nodules.
- removal of all or part of the gland due to malfunction, uncontrolled by medical treatment.
- remove all or part of the gland because of its size and the risk of compressing neighbouring structures
- prevent cancer in cases of proven genetic risk (family history of multiple endocrine neoplasia)
REALIZATION OF THE INTERVENTION
This procedure is usually performed under general anesthesia. The skin incision is horizontal, located in the lower and middle part of the neck, if possible in a natural skin fold, and the length of the incision is adapted to the type of procedure and the volume of the gland (goiter).
Depending on the type of intervention proposed, we will carry out :
- removal of an isolated nodule (enucleo-resection),
- lobo-isthmectomy, i.e. removal of half your thyroid gland,
- subtotal thyroidectomy,
- total thyroidectomy.
Tissue analysis under a microscope of the nodule(s) may be requested during the operation (extemporaneous examination, with immediate analysis, but the result is not definitive and is not 100% reliable), in order to clarify the nature of the tumour and modify the extent of the surgical procedure. In the case of malignant tumours, total thyroidectomy is the rule, and will be associated with removal of lymph nodes in the neck region and along the trachea, depending on the initial work-up. The surgical incision will need to be enlarged if the lymph nodes on the sides of your neck are to be removed. One or more drains will usually be inserted, depending on the extent of the surgical intervention.
Hospitalization lasts 2 days, necessary to remove the drain. Pain is slight, essentially due to the prolonged position of the head in extension after the operation.
An intradermal overlock thread is removed after 8 days.
OPERATING RISKS
First and foremost, the neck hematoma may need to be evacuated again, as the hematoma compresses the trachea and may impair breathing.
In the event of total thyroidectomy, cramps and tingling in the hands and feet may occur, due to dysfunction of the para-thyroid glands and a drop in blood calcium levels. These disorders are usually transient and require medical treatment.
The main risk is trauma to the recurrent nerve (responsible for mobility of the vocal cords), which can lead to voice disorders that are usually transient and may require temporary rehabilitation. These voice disorders may be accompanied by swallowing problems and breathing difficulties on exertion. - Breathing disorders: these can be serious, requiring ventilatory assistance, or even tracheostomy or laryngeal surgery. Exceptional complications include tracheal necrosis in the case of total thyroidectomy, and lymph leakage in the case of associated lymph node surgery.
CHRURGICAL CONSEQUENCES:
Total or near-total removal of the thyroid gland requires lifelong replacement therapy to compensate for the absence of hormone secretion. In the event of partial removal of the thyroid gland, thyroid secretion should be monitored by a biological test carried out at a distance from the operation (depending on the results, hormone therapy may be prescribed).
The scar may show adhesions or become thickened.
.JPG)

